The practical differences between PCV & VCV

This chapter vaguely addresses the requirements of the CICM WCA document (“Ventilation”), where a successful trainee “outlines the differences between volume and pressure controlled ventilation”. The definition of control variables and the very flimsy definition of “control” are discussed in a chapter which is dedicated to such puffery, left out of this chapter and put aside so that serious discussion can take place here. There are some substantial differences between the conventional pressure control and volume control modes, which are mainly related to the shape of the pressure and flow waveforms which they deliver.
In summary:
In general, volume control favors the control of ventilation, and pressure control favors the control of oxygenation.
Volume and pressure control modes have distinct advantages and disadvantages which are mainly related to the flow and pressure patterns of gas delivery.
Volume control:
o Advantages:
§ Guaranteed tidal volumes produces a more stable minute volume
§ The minute volume remains stable over a range of changing pulmonary characteristics.
§ The initial flow rate is lower than in pressure-controlled modes, i.e. it avoids a high resistance-related early pressure peak
o Disadvantages:
§ The mean airway pressure is lower with volume control ventilation
§ Recruitment may be poorer in lung units with poor compliance.
§ In the presence of a leak, the mean airway pressure may be unstable.
§ Insufficient flow may give rise to patient-ventilator dyssynchrony.
Pressure control:
o Advantages:
§ Increased mean airway pressure
§ Increased duration of alveolar recruitment
§ Protective against barotrauma
§ Work of breathing and patient comfort may be improved
o Disadvantages:
§ Tidal volume is variable and dependent on respiratory compliance
§ Uncontrolled volume may result in “volutrauma“ (overdistension)
§ A high early inspiratory flow may breach the pressure limit if airway resistance is high.
Adaptive control modes combine the advantages of pressure and volume control modes without the disadvantages
A good example of an adaptive control mode of ventilation is PRVC, which guarantees a prescribed volume while maintaining a square pressure waveform and therefore a high mean airway pressure.
One disadvantage of the adaptive control targeting schema is that the mean airway pressure will be somewhat variable, depending on compliance and patient effort.
Pressure control modes of ventilation
In a pressure controlled mode of ventilation, the inspiratory pressure is the control variable, and is maintained during the inspiratory phase. As a result of this, the pressure waveform is “square”. This increases the mean airway pressure (i.e. the area under the pressure/time graph is greater).
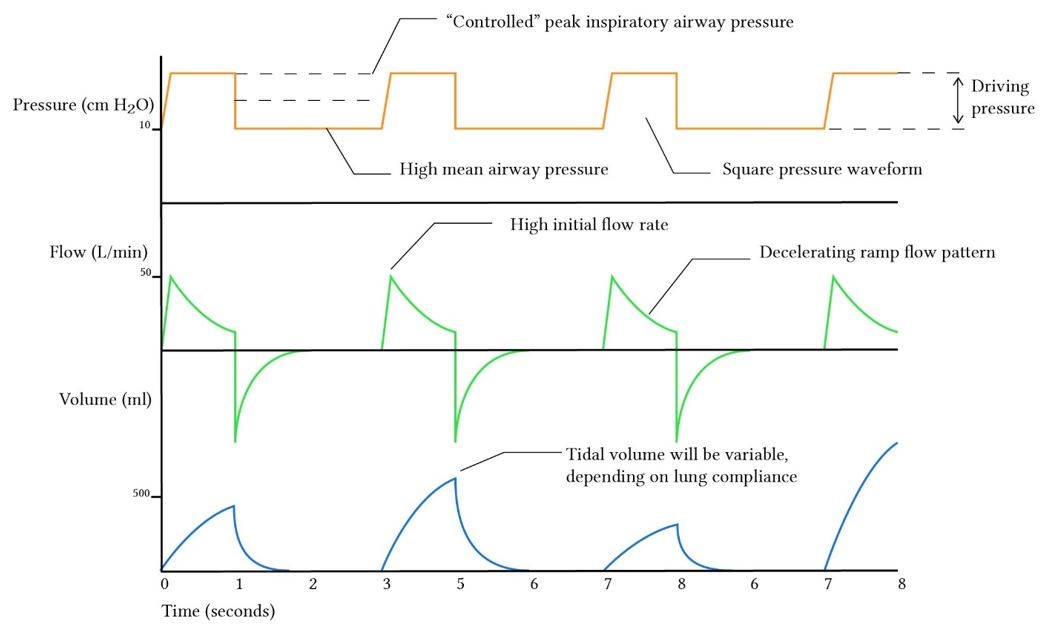
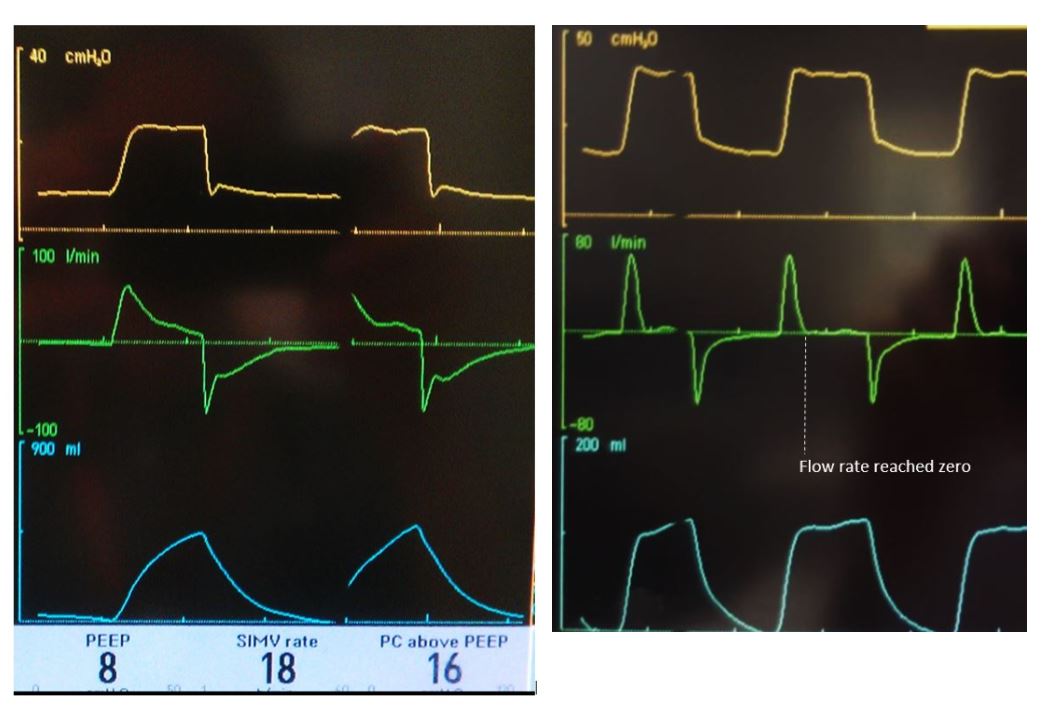
During the early inspiratory phase, the ventilator provides a high inspiratory flow rate to rapidly achieve the pressure limit variable ("PC above PEEP" on a SERVO-I). In order to maintain this pressure, the flow rate needs to decrease over the course of inspiration, and it generally takes the shape of a down sloping ramp. If the inspiratory time is long enough, the flow will eventually reach zero, as demonstrated in the ventilator graphic below. When the flow rate reaches zero, i.e. in the absence of flow, the constant prescribed pressure is in equilibrium with the peak alveolar pressure at the end of the breath and equals the plateau pressure.
Advantages of PCV
PCV has a series of theoretical advantages in ventilating a patient in whom hypoxia and poor lung compliance are major contributors to respiratory failure:
· Increased mean airway pressure, which improves oxygenation (as discussed elsewhere the mean airway pressure is one of the main determinants of the oxygenation improvement associated with positive pressure ventilation). Because the dominant influence on mean airway pressure is PEEP, this is not a massive advantage until you start using extremely inspiration-heavy I:E ratios, e.g. 1:1.5 or 1:1
· Increased duration of alveolar recruitment: with a square pressure waveform, alveoli are opened earlier and remain open for longer, allowing better gas exchange (i.e. the early high airway pressure allows the alveoli to benefit from the high pressure for longer)
· Pressure limited ventilation may protect against barotrauma; the fixed pressure level defends against pressure-induced alveolar injury. In other words, because the pressure level is controlled, there should never be a time where the patient is suffering from extremely high pressures.
· Work of breathing and patient comfort may be improved because the initial high flow rate prevents the "flow starvation" type of patient-ventilator dyssynchrony, where the patient's demand for fresh gas flow goes unmet by the ventilator's inappropriately low flow limit. Cinella et al (1996) found that this was the case at low-moderate tidal volumes, i.e. wherever the pressure control mode competes with a volume control mode which is set to low flow, the patient’s work of breathing will be better with a square pressure waveform.
Additionally, the pressure control variable allows for a significant leak. The ventilator will automatically adjust the inspiratory flow rate to accommodate for even a significant leak in an effort to maintain the prescribed pressure level. This has advantages in settings where circuit leak is inevitable, for example during bronchoscopy or while ventilating a patient with a bronchopleural fistula.
Disadvantages of PCV
· Tidal volume is dependent on respiratory compliance; and it may vary substantially over the course of mechanical ventilation, requiring frequent adjustments. With PCV, without constant attention to the ventilator settings tight control of PaCO2 may be difficult to achieve.
· Uncontrolled volume may result in volutrauma, i.e. if the lung compliance improves suddenly the ventilator may deliver volumes which distend the most compliant lung units beyond their elastic limit.
· A high early inspiratory flow may breach the pressure limit if airway resistance is high. The high initial flow rate will create a high pressure due to airway resistance, which could be high enough to blow the pressure alarm limit. If airway resistance is a problem, a more gentle inspiratory flow rate might be beneficial.
Volume control modes of ventilation
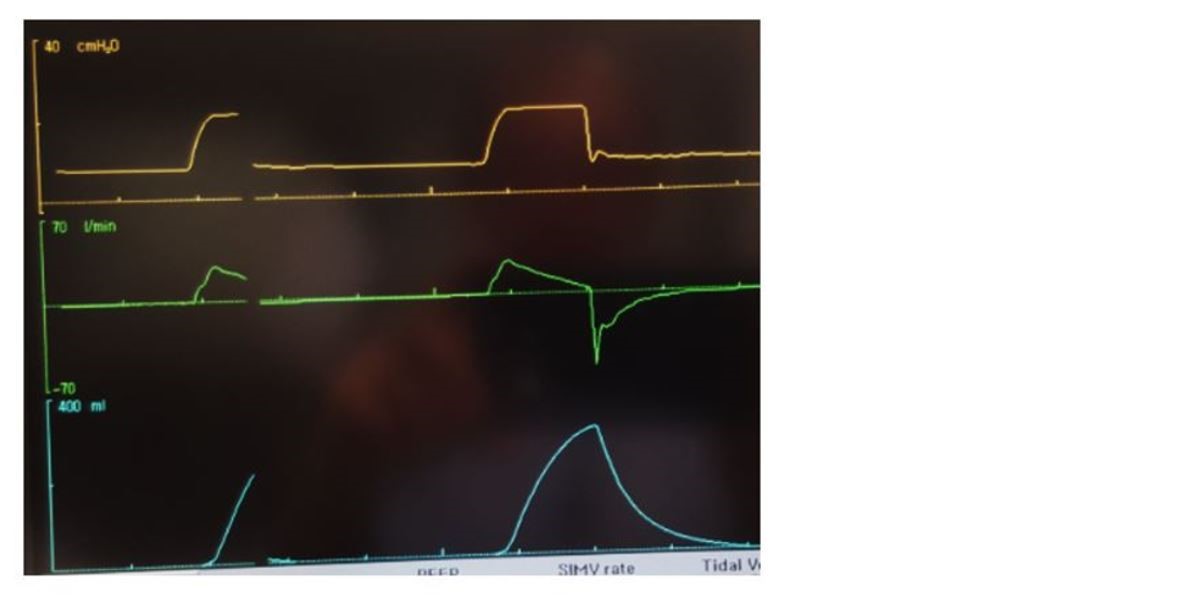
By definition, in volume control modes the tidal volume is the defined variable which is used by the ventilator to give feedback to the solenoid valve circuits. As volume and flow are inextricably linked, the volume control modes are generally constant flow modes, i.e. the ventilator delivers flow which is constant, and stops this flow when the desired volume is achieved. Because pressure is not controlled or regulated in any way, the pressure waveform takes a parabolic sloping shape as the lungs distend during a breath.
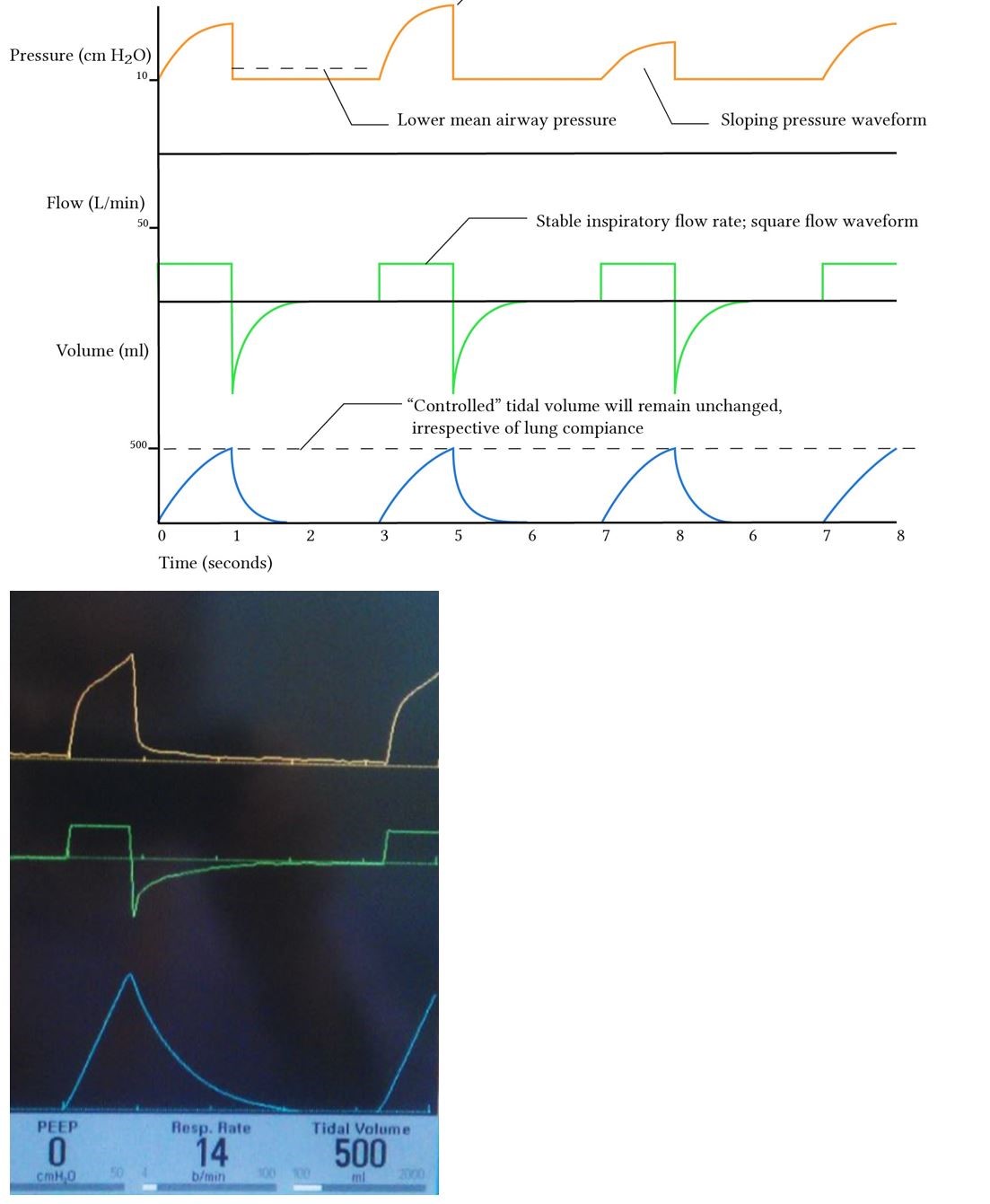
The pressure waveform is highly variable during volume control ventilation, changing shape depending on lung compliance and airway resistance. As a result, it offers a significant amount of information. Interpretation of the pressure waveform is discussed elsewhere.
Advantages of volume control ventilation
· Guaranteed tidal volumes produce a more stable minute volume. The reliability of the minute volume makes this mode of ventilation more appropriate in situations where careful control of PaCO2 is of importance. Volume controlled modes were the standard of care for patients with severe traumatic brain injury where tight PaCO2 control is necessary.
· The minute volume remains stable over a range of changing pulmonary characteristics. If airway resistance fluctuates significantly (e.g. in the course of therapy for status asthmatics) this mode has the advantage of maintaining a reliable minute volume.
· The initial flow rate is lower than in pressure-controlled modes. This is an advantage if airway resistance is high; blowing more slowly into the tight bronchi does not produce a high resistance-related early pressure peak, and potentially prevents an early termination of the breath by the pressure alarm limit.
Disadvantages of volume control ventilation
· The mean airway pressure is lower with volume control ventilation, due to the slopy shape of the pressure waveform. This can theoretically be a disadvantage in patients who have severe hypoxia in those people one might want to use a pressure-controlled mode instead. One way of getting around this is to use an inspiratory pause, which is discussed elsewhere (in summary, it doesn’t work and possibly increases the work of breathing).
· Recruitment may be poorer in lung units with poor compliance. Units with a long time constant and poor compliance may remain unrecruited until very late in the inspiratory phase when pressure approaches its maximum value. These units will have little time for gas exchange before the ventilator cycles to expiration. From this, one might expect that with a volume-controlled mode the degree of atelectasis will be greater than with a pressure controlled mode, peak airway pressures being equal.
· In the presence of a leak, the mean airway pressure may be unstable. The constant flow used during VCV may not be able to compensate for an intermittent leak. Consider: if the leak flow rate is equal to the inspiratory flow rate, there will be no volume delivered.
· Insufficient flow may give rise to patient-ventilator dyssynchrony. In the presence of increased respiratory demand during the course of a breath, the ventilator may not meet the patient's need for increased flow.
Scenarios where the choice of control variable matters
The evidence which supports the specific choice of a pressure control mode or volume control mode is surprisingly scant, prompting authors such as Campbell and Davis (2002) to publish articles titled something like “Pressure-controlled versus volume-controlled ventilation: does it matter?” (Spoiler: it doesn’t). This should not be viewed negatively as uncertainty or disagreement among experts. A better way to put it would be to borrow a turn of phrase from the narrative review by Rittayamai et al (2015), who reviewed the conflicting literature and concluded triumphantly that “these data should help to open the choice of ventilation of patients with acute respiratory failure”. In short, because there is no obvious winner, anything goes – you’ll not be criticized for using either mode. With that said, it is possible to discuss the few scenarios where PCV and VCV were compared directly. The literature understandably focuses on ARDS, and inexplicably on bariatric surgery and one-lung ventilation.
In ARDS, though the teaching is to use a pressure-controlled mode, the evidence for this is weak. For example, Lessard et al (1994) compared volume and pressure controlled modes with a variety of I:E ratios, and came to the conclusion that there was no short-term beneficial effect of PCV. In fact with inverse ratio ventilation PCV (I:E 2:1) there was a deterioration of oxygenation, in spite of higher mean airway pressure. One cannot help but think that they may have needed to fill that patient with more volume. Esteban et al (2000) randomized about 40 patients to VCV or PCV and found a preposterous-sounding mortality difference (78% vs 51%) in favor of pressure control, which is difficult to take seriously because the group mortality is well in excess of the norm, suggesting something biased the result (the authors themselves conclude that “the development of organ failures was probably not related to the ventilator mode”). There are a ton of such small contradictory trials. Looking at things through the Cochrane telescope, Chacko et al (2015) rounded up over 1000 patients from three good-sized RCTs and concluded soberly that the available data are “insufficient to confirm or refute” the standing hypothesis. As things stand,
In one-lung anesthesia, there may be some benefit to pressure control, over volume control. Tugrul et al (1997) found that oxygenation improved and peak airway pressures decreased during one-lung ventilation. Unzueta et al (2007) agreed that peak pressures were lower, but did not replicate the improved oxygenation.
In laparoscopic obesity surgery, pressure control seems to have an advantage (Cadi et al, 2008). Surprisingly, when the mean airway pressure was calculated for these patients, there was not significant difference between groups. The authors suggested that the high early flow rate in PCV somehow contributes to some sort of “instantaneous regional pressures” in the lungs, implying that the overdistension of short time-constant alveoli is responsible for the improved gas exchange
Dual control and adaptive control modes
Acknowledging the major disadvantages of the abovementioned modes of ventilation, adaptive modes such as PRVC are a fusion of the two strategies which combines the advantages of each without magnifying their disadvantages. For a PRVC mode, the user sets a target tidal volume, as in a volume control mode. The Maquet SERVO-I then performs an assessment of the dynamic lung compliance over the course of three initial calibrating breaths, which are volume control breaths. Using this lung compliance data, it then determines the appropriate pressure level required to achieve the prescribed tidal volume.
This mode does have some disadvantages: a variable patient effort may lead to a highly variable tidal volume, because the pressure level is dependent on the respiratory characteristics over the previous breaths. However, it preserves several advantages of PCV and VCV, and none of their disadvantages:
· Square pressure waveform favors early and sustained lung unit recruitment
· Mean airway pressure is as high as with PCV
· Pressure is minimized for any given prescribed tidal volume
· A minute volume is guaranteed, preserving a degree of control over PaCO2
The decelerating flow waveform seems to be the main determinant here. By using this pattern of flow, volume controlled modes lose many of their disadvantages. For example, Davis et al (1996) found that whenever they used a decelerating ramp flow waveform, their patients were well-oxygenated irrespective of whether they used volume or pressure as the control variable.


